CENTRIVIVE significantly
reduces Death and Disability
within first 90 days of its use
in Acute Ischemic Stroke (AIS)

About Acute Ischemic Stroke (AIS)
What is stroke?
Stroke is the second-leading cause of death (11.6% of total deaths) and the third-leading cause of death and disability combined (5.7% of total disability adjusted life years (DALYs)). The economic cost of stroke is staggering, not only does recovery require complex and lengthy medical interventions and rehabilitation, but it also causes a significant loss of productivity.
Ischemic stroke accounts for 70%-80% of total prevalence of stroke. Less than 2% patients reach stroke care unit within golden period and mortality rate is generally lower in such cases. First 90 days post stroke poses a highest risk in terms of mortality and disability. It is estimated that around 30%-40% people with stroke die in first 90 days.
Remaining 60% suffer from post stroke disabilities and disorders like -
Post Stroke Fatigue Post Stroke Depression Post Stroke Cognitive Impairment Post Stroke Chronic Neuropathy Vascular Dementia

Need of the hour is to ensure reperfusion to ischemic areas. Neovascularisation is considered as a novel strategy to restore blood supply to the ischemic brain tissues.
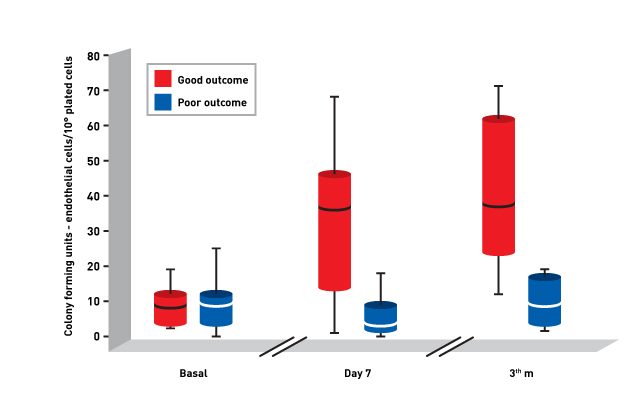
American stroke association (Stroke : 2007; 38;2759-2764) published a study establishing relationship between circulating endothelial progenitor cells (EPCs) and prognosis of acute ischemic stroke. Circulating endothelial progenitor cells (EPC), which derive from bone marrow and move to the peripheral blood, have been suggested to be a marker of cardiovascular risk and endothelial function.
The number of circulating EPC has been reported to be decreased in patients with cardiovascular risk factors such as smoking habit, hypercholesterolemia, diabetes and hypertension, many of which have been identified as prognostic markers of poor outcome after ischemic stroke.

Moreover, low EPC number has also been found in patients with unstable angina and cerebrovascular disease.
Study concluded that EPC have been involved in repair processes and are associated with improved functional outcome and reduced brain injury in patients with acute ischemic stroke.
Figure: Temporal profile of median (qualities) CFU-EC number in patients with good or poor outcome at 3 months.